Ovarian cancer
Malignant tumor arising from ovarian tissue. Epithelial ovarian carcinoma is by far the most common (~90%), but ovarian cancer also includes germ cell tumors and sex cord–stromal tumors with distinct behaviors.
- Ovarian cancer is the deadliest gynecologic malignancy due to late presentation. It's a high-yield topic because of its vague symptoms, unique tumor markers (CA-125, AFP, β-hCG, etc.), and the need to distinguish subtypes (epithelial vs germ cell vs stromal) on exams.
- Often in a postmenopausal woman with vague GI symptoms: abdominal bloating, early satiety, pelvic or abdominal pain, urinary urgency. Exam may reveal a palpable adnexal mass and possibly ascites. CA-125 is often elevated.
- Young women or teens with a rapidly enlarging pelvic mass. May present with acute pain from torsion or rupture. Tumor markers can be positive (e.g., ↑AFP in yolk sac tumor, ↑β-hCG in choriocarcinoma or embryonal carcinoma, ↑LDH in dysgerminoma).
- Findings of hormone production: e.g., an ovarian mass with estrogen effects (precocious puberty in a girl, or endometrial hyperplasia/postmenopausal bleeding in an older woman) suggests a granulosa cell tumor; virilization (hirsutism, deep voice) suggests a Sertoli-Leydig cell tumor.
- Always consider patient age. An adnexal mass in a younger patient → evaluate for germ cell tumor (AFP, β-hCG, LDH). In a postmenopausal patient → high suspicion for epithelial carcinoma (CA-125).
- Use transvaginal ultrasound (TVUS) to characterize any ovarian mass. Benign features: simple, unilocular cyst <5 cm, smooth walls. Suspicious features: solid or complex mass, thick septations, bilateral masses, or ascites.
- If malignancy is suspected, obtain appropriate imaging (CT scan of abdomen/pelvis +/- chest) for extent, and refer to a gynecologic oncologist for surgical management. Avoid simple cyst aspiration—if the mass is cancer, spillage can spread tumor cells.
- Check tumor markers preoperatively to guide the differential: CA-125 (especially if postmenopausal), CEA/CA19-9 (mucinous or GI origin), AFP, β-hCG, LDH (if germ cell tumor suspected), Inhibin (granulosa cell tumor). These help narrow the diagnosis but are adjuncts, not definitive.
| Condition | Distinguishing Feature |
|---|---|
| Tubo-ovarian abscess | PID history, fever and pelvic pain; inflammatory adnexal mass (responds to antibiotics) |
| Endometrioma | "Chocolate cyst" from endometriosis; premenstrual pelvic pain; "ground-glass" appearance on ultrasound |
| Mature cystic teratoma | Benign dermoid cyst; young women; often contains fat or calcifications (teeth) on imaging |
- Primary treatment is surgical. For epithelial ovarian cancer, perform surgical staging and debulking: remove the uterus, both ovaries and tubes (TAH-BSO), omentum, and any visible tumor nodules. Goal is to leave no macroscopic disease. (In early-stage young patients wishing fertility, unilateral oophorectomy can be considered if disease is limited.)
- Nearly all patients will need platinum-based chemotherapy after surgery. Standard regimen for epithelial ovarian carcinoma is combined carboplatin + paclitaxel. For malignant germ cell tumors, use BEP chemo (Bleomycin, Etoposide, Cisplatin), which yields high cure rates. Sex cord-stromal tumors may also receive chemo (often using BEP) if high stage or poorly differentiated.
- Advanced or high-risk cases often get maintenance therapy after chemo. Examples: Bevacizumab (anti-angiogenic) is often added for stage III-IV disease, and PARP inhibitors (like olaparib) are used especially in patients with BRCA mutations or homologous recombination deficiency to prolong remission.
- Always involve a gynecologic oncology specialist for suspected ovarian cancer. Appropriate surgical staging and cytoreduction by an expert improves outcomes. In younger patients with malignancy who desire fertility, a fertility-sparing approach (removing only the affected ovary, if early stage) can be done, followed by chemo, with careful follow-up.
- Use the mnemonic "BEAT" for common ovarian cancer symptoms: Bloating, Early satiety, Abdominal pain, Trouble with bladder (urinary urgency). These vague complaints in an older woman should raise concern for ovarian cancer.
- Don't confuse ovarian cancer with Meigs syndrome: a benign ovarian fibroma with ascites and pleural effusion. Meigs can mimic cancer (mass + ascites) but resolves after fibroma removal.
- Postmenopausal woman with any adnexal mass or unexplained ascites is a red flag for ovarian malignancy until proven otherwise – prompt evaluation and referral is warranted.
- CA-125 level very elevated (e.g. >200 U/mL, especially in a postmenopausal patient) strongly suggests an ovarian cancer (though moderate elevations can occur in benign conditions).
- An ovarian mass with acute torsion or rupture can be life-threatening (severe abdominal pain, peritonitis). While not a "malignancy" sign per se, any patient with known ovarian mass who develops sudden severe pain needs emergency surgical assessment (masses >5 cm increase torsion risk).
- Patient presents with possible adnexal mass (e.g., pelvic exam finding or symptoms) → Transvaginal ultrasound for characterization.
- If ultrasound suggests a benign cyst (small, simple, likely functional) and patient is low-risk → observe and follow up imaging; consider elective laparoscopic cystectomy if persistent or symptomatic.
- If ultrasound or clinical factors are suspicious for malignancy (solid components, septations, nodularity, ascites, or patient is postmenopausal) → Measure tumor markers (e.g., CA-125) and obtain cross-sectional imaging (CT scan) as needed → Refer to gynecologic oncology before intervention.
- Proceed to surgical exploration for definitive diagnosis and treatment. Perform appropriate cancer staging surgery (with frozen section guidance intra-op). If malignancy is confirmed, execute debulking and then plan for adjuvant chemotherapy. If benign, manage accordingly (cystectomy or oophorectomy as needed).
- A 63-year-old woman with increasing abdominal girth, early satiety, and an adnexal mass on exam. Ultrasound shows a solid complex ovarian mass with ascites; CA-125 is markedly elevated → Epithelial ovarian carcinoma (likely high-grade serous).
- An 18-year-old woman with an acute abdominal pain and pelvic mass. Serum AFP is high (or β-hCG is high) → Ovarian germ cell tumor (e.g., yolk sac tumor if AFP, choriocarcinoma if β-hCG). Tumor is often unilateral and rapidly enlarging.
- A postmenopausal woman with a thickened endometrium, postmenopausal bleeding, and an ovarian mass → think granulosa cell tumor (estrogen-secreting sex cord–stromal tumor causing endometrial hyperplasia/carcinoma).
A 62-year-old woman reports progressive abdominal bloating, early satiety, and pelvic discomfort for 2 months. She also notes her pants fitting tighter due to a "swollen belly." On exam, she has a distended abdomen with a fluid wave and a firm, fixed right adnexal mass. CA-125 level is 560 U/mL (normal <35).
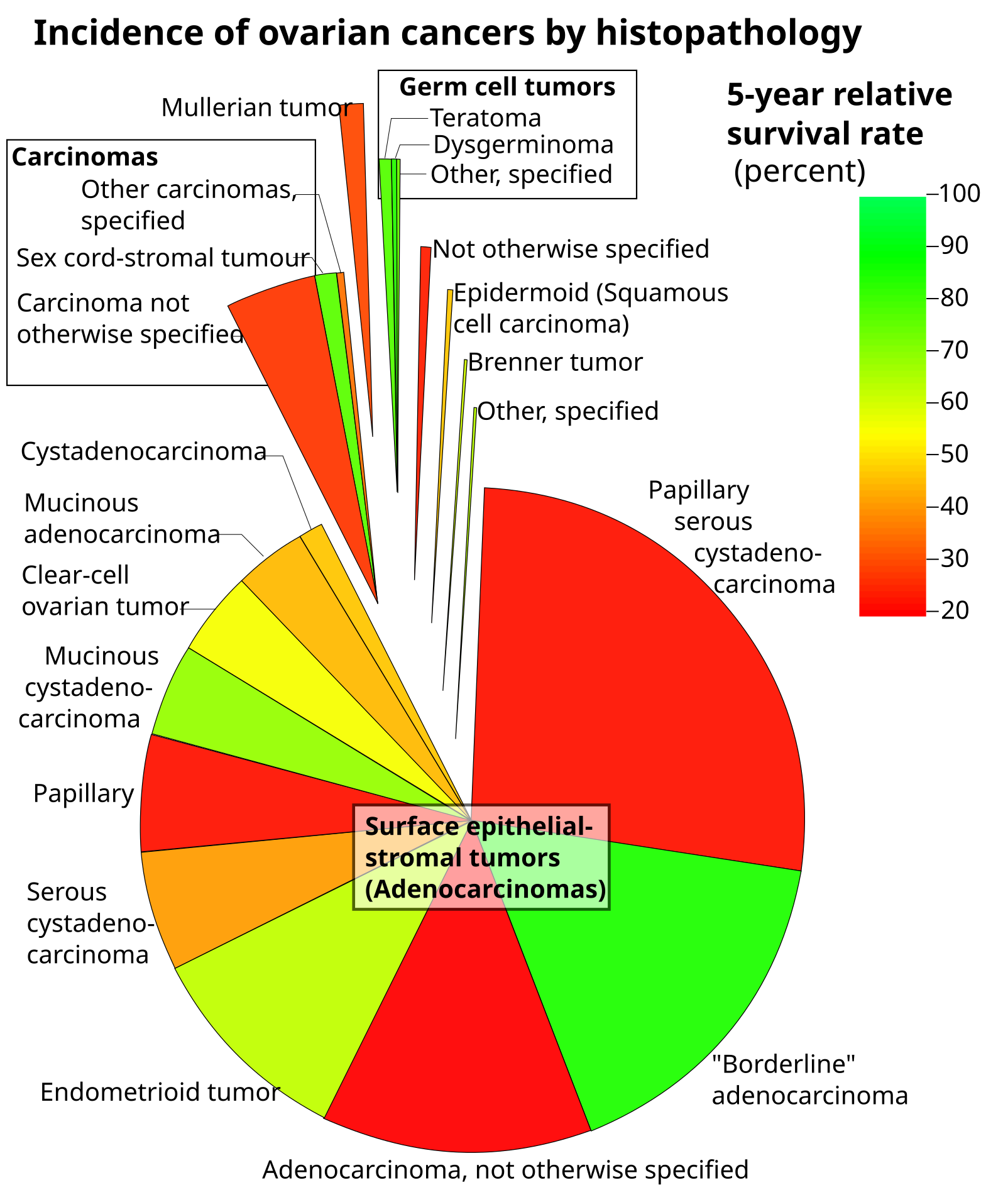
Chart illustrating ovarian cancer subtypes by histology (area of each segment correlates with frequency, and color indicates 5-year survival rate: green for higher survival, red for lower). Epithelial tumors (large red segment) account for the vast majority of ovarian cancers.
image credit📚 References & Sources
- 1JAMA: Ovarian Cancer – A Review (Caruso et al., 2025)
- 2StatPearls: Epithelial Ovarian Cancer (Ray-Coquard & Westin, updated 2024)
- 3UpToDate: Overview of Epithelial Ovarian Cancer (Chua & Chu, 2023)
- 4NCCN Guidelines Insights: Ovarian Cancer, Version 3.2022 (Morgan et al., 2022)
